With some political leaders calling for the US to move to Medicare-for-all and California weighing a proposal to have all patient care reimbursed at Medicare rates, it is worth taking a step back to examine the level of traditional Medicare’s provider payment rates. Specifically, do the current payment rates ensure high quality and access for Medicare beneficiaries, while keeping high-value providers in business. Our review of the latest MedPAC report to Congress and statements made by the Medicare Actuary paints a pretty grim picture, as far as delivering on the above objectives.
The March, 2018 MedPAC report shows that aggregate hospital margins from Medicare have gone from -4.9% in 2010 to -9.6% in 2016, and are projected to be -11% in 2018. It is of interest to note that MedPAC looks only at Medicare ‘allowed’ costs – which removes many other expenses incurred by hospitals such as private rooms for patients, telephones and TVs in patient rooms, marketing communications, interest on certain borrowed funds, etc. Thus, true Medicare margins, that are based on total costs, are actually worse than those reported by MedPAC.
Low Medicare payment rates and their implications for both beneficiaries and providers have also been the subject of repeated commentary by the Medicare Actuary, e.g.,
- “Limiting (Medicare) cost growth to a level below inflation would represent an exceedingly difficult challenge… Providers for whom Medicare constitutes a substantial potion of their business…might end their participation in the program”
- “…the prices paid by Medicare for most health services will fall increasingly short of the cost of providing such services. If this issue is not addressed by subsequent legislation, it is likely that access to, and quality of, Medicare benefits would deteriorate over time for beneficiaries.”
The CMS Maryland experience
So, how can we estimate the true magnitude of the problem with current Medicare provider payment rates? One state in the US, Maryland, has had all payer rate setting for over 40 years. The Health Services Cost Review Commission (HSCRC), an independent agency established by the Maryland legislature in the early 1970s, is charged with setting uniform hospital service rates. As such, all Maryland payers are charged the same rates approved by the commission (with a modest discount allowed for Medicare and Medicaid). While Maryland can certainly work on improving efficiency (and is moving in that direction with the recent transition to global budgets), one would presume that the present rates are set to meet the following goals of the commission:
- “Ensure that hospitals have the financial ability to provide efficient, high quality services to all Marylanders
- Increase the equity or fairness of hospital financing”
If the above presumption is true, then Maryland’s all payer rates can shed light on the adequacy of traditional Medicare’s payment rates to accomplish the same two objectives.
Fortunately, CMS-commissioned evaluation reports of the Maryland All-Payer Model have done some detailed work on this particular topic. Specifically,
- “The analyses compared the weighted average payment per inpatient admission in Maryland and a comparison group for the same mix of admissions… also examine the weighted average payment per hospital outpatient visit. Using the same mix of admissions and hospital outpatient visits controls for utilization differences between Maryland and the comparison group so the comparison only reflects payment rate differences.”
The latest evaluation report shows that between 2011 and 2016, Maryland Medicare rates for inpatient admissions were 33-40% higher than in the comparison group paid at traditional Medicare rates. The payment gap was even wider for outpatient hospital services, with Maryland Medicare payment rates (FY2013-2016) coming in at 55-62% higher than those of the matched comparison group paid at traditional Medicare payment rates. Clearly, the present policies of increasing traditional Medicare payment rates by less than inflation, have created a major Medicare payment shortfall, which (absent major changes) will get even bigger in the coming years. The rate gap further suggests that the under age 65, privately insured patient population, is currently subsidizing the care of Medicare beneficiaries. Thus, trying to put all patients on traditional Medicare payment rates would make the Medicare Actuary’s worrisome conclusions even more dire. Conversely, assuming Maryland is doing a good job setting payment rates, going to Medicare-for-all using the Maryland model, would require massive increases in rates over what Medicare presently pays everywhere else. Unless there was a change in provider efficiency, there would need to be ~40% increase in what Medicare pays for inpatient admissions and ~60% increase in payment for outpatient hospital services.
Medicare payment policies could benefit from a major overhaul
Based on the various sources of evidence presented above, we believe that Medicare payment rates are too low and getting worse every year. That said, we also believe that it is incumbent on the delivery system to improve efficiency and thus get better value. While providers would certainly welcome increases in Medicare payment rates, changes in payment rates alone will not be sufficient to drive improvement in healthcare delivery.
As we think about what providers should be paid, it would behoove us to remember a Commonwealth Fund blog by Dr. Stuart Guterman and others, which stated that: “… payment levels must be carefully calibrated to ensure providers’ financial viability while providing incentives to reduce costs and safeguards to ensure high quality.” Unfortunately, our conclusion is that traditional Medicare payment rates and policies fall short of the Commonwealth Fund recommendations. The financial viability of the US healthcare provider depends heavily on private payers (and thus the younger and employed population), while traditional Medicare is characterized by wide variation in service utilization, costs, and patient outcomes.
We believe that accomplishing the objectives described by Guterman et al., can best be accomplished by payment structures that ensure the financial viability of high value providers – those getting better patient outcomes at lower than average costs. In turn, the rates should be based on the real costs of doing business by these highest value providers (and not what Medicare currently pays them) plus a 2-4% margin, since even non-profit organizations need reserves to address changing staffing needs, replace aging equipment, etc. With regard to the need for a positive margin by providers, it is of interest to note that the Maryland HSCRC agrees. It has established hospital profitability targets of 2.75% operationally and a 4% total margin.
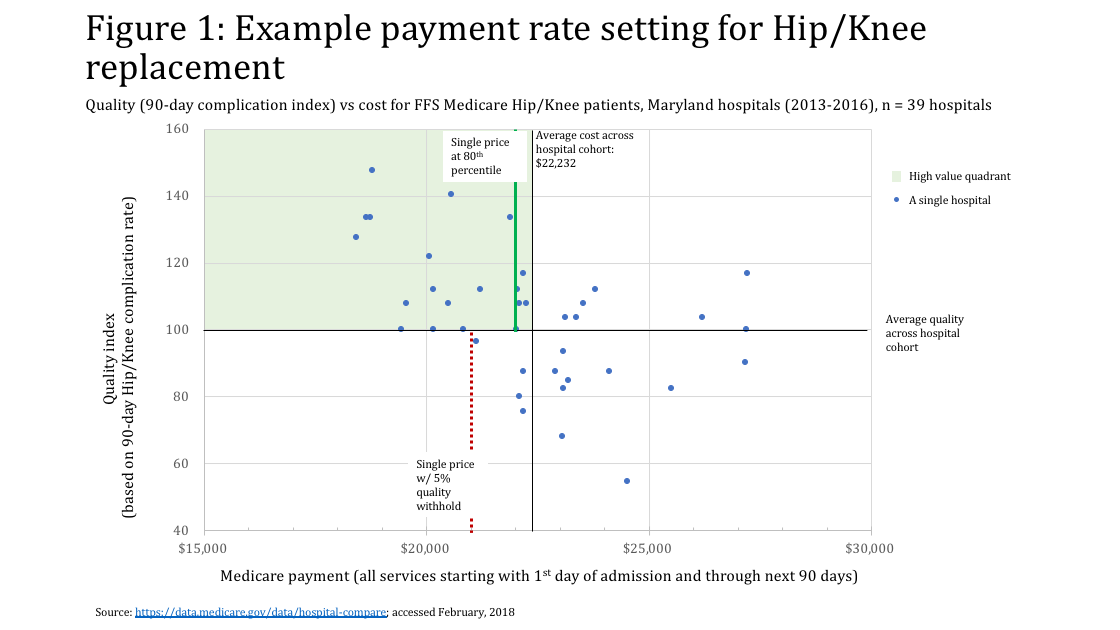
While we have detailed such value-based payment approaches in previous publications, it may be worth re-iterating a couple of the key components. Again, taking the state of Maryland as an example, Figure 1 shows the distribution of risk-adjusted quality index (based on the 90-day complication rate for hip/knee replacement) vs. the corresponding cost per episode of care. A base payment rate could be set at the 80thor 90thpercentile of the delivery organizations that are in the high value quadrant (i.e., those that get better than average quality at lower than average cost). A further quality withhold (e.g., 5%) could be used to ensure that providers don’t sacrifice effectiveness in the name of efficiency or that we do not reward low quality providers for simply being low cost. HSCRC has an objective establishing “rates sufficient to meet ‘full financial requirements’ of efficient/effective hospitals.” The pay for value approach we outlined above would create a strong incentive for providers to move to high value. If we truly desire a high value healthcare delivery system, we would be more likely to get it, if we actually paid for value.
Excellent piece – and the last sentence is so critically important.
“The pay for value approach we outlined above would create a strong incentive for providers to move to high value. If we truly desire a high value healthcare delivery system, we would be more likely to get it, if we actually paid for value.”
Denis and Bob:
A great reminder that the Medicare for All advocates do not really understand the financial implications of their aspirations…there also is a hope that administrative savings will arise as marketing, customer service and claims processing needs diminish–really? Hope your summer going well…keep the conversation going…